Clinical characteristics and time of initiation of thrombolytic treatment in patients with Ischemic Cerebrovascular Accident in the Stroke Unit of the Emergency Service of the Hospital de Clínicas
Main Article Content
Abstract
Introduction: intravenous thrombolysis revolutionized the therapy of patients with ischemic strokes.
Objective: to determine the clinical characteristics and time of initiation of thrombolytic treatment in patients with ischemic stroke in the Stroke Unit of the Hospital de Clínicas.
Methodology: this was a retrospective, observational, descriptive, cross-sectional study, we used non-probabilistic sampling, of patients with a diagnosis of ischemic stroke admitted to the Stroke Unit of the Hospital de Clínicas, from January 2015 to June 2022. Sociodemographic variables, start time of thrombolytic treatment, NIHSS at admission, 24 hours and 5 days, ASPCT scale, glycemia, systolic and diastolic blood pressure, risk factors for heart disease, hemorrhagic transformation.
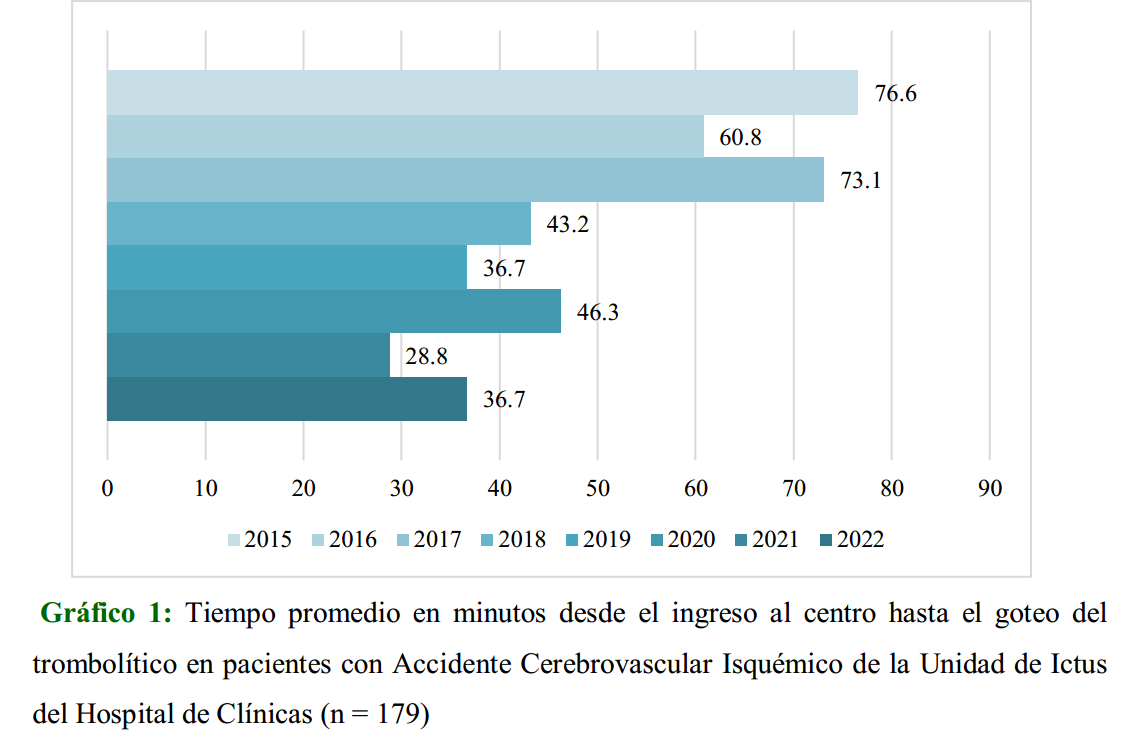
Results: 10 % of patients met thrombolysis criteria, with a mean age of 62 ± 1,59 % were male. The average time from hospital admission to the thrombolytic drip was 44 ± 2 minutes and from the onset of symptoms to the thrombolytic drip was 195 ± 5 minutes. The most frequent cardiovascular risk factors were High Blood Pressure and Diabetes Mellitus; symptomatic hemorrhagic transformations occurred in 5 % of the thrombolyzed patients.
Conclusion: 10 % of patients met criteria for thrombolysis. The mean time from hospital admission to the fibrinolytic drip was 44 minutes and from the onset of symptoms to the thrombolytic drip was 195 ± 5 minutes. The most frequent risk factors for heart disease were High Blood Pressure and Diabetes Mellitus, 5 % of symptomatic hemorrhagic transformation occurred.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Usted es libre de:
- Compartir: copiar y redistribuir el material en cualquier medio o formato para cualquier propósito, incluso comercialmente.
- Adaptar: remezclar, transformar y construir a partir del material para cualquier propósito, incluso comercialmente.
- La licenciante no puede revocar estas libertades en tanto usted siga los términos de la licencia
Bajo los siguientes términos:
- Atribución: Usted debe dar crédito de manera adecuada, brindar un enlace a la licencia, e indicar si se han realizado cambios. Puede hacerlo en cualquier forma razonable, pero no de forma tal que sugiera que usted o su uso tienen el apoyo de la licenciante.
- Compartir igual: — Si remezcla, transforma o crea a partir del material, debe distribuir su contribución bajo la misma licencia del original.
- No hay restricciones adicionales — No puede aplicar términos legales ni medidas tecnológicas que restrinjan legalmente a otras a hacer cualquier uso permitido por la licencia.
References
Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int J Stroke. 2022;17(1):18-29. doi: 10.1177/17474930211065917
Gu HQ, Yang X, Wang CJ, Zhao XQ, Wang YL, Liu LP, et al. Clinical characteristics, management, and in-hospital outcomes in patients with stroke or transient ischemic attack in China. JAMA Network Open. 2021;4(8):e2120745. doi: 10.1001/jamanetworkopen.2021.20745.
LeCouffe NE, Kappelhof M, Treurniet KM, Rinkel LA, Bruggeman AE, Berkhemer OA, et al. A randomized trial of intravenous alteplase before endovascular treatment for stroke. N Engl J Med. 2021;385(20):1833-1844. doi: 10.1056/NEJMoa2107727
Lyden S, Wold J. Acute Treatment of Ischemic Stroke. Neurol Clin. 2022;40(1):17-32. doi: 10.1016/j.ncl.2021.08.002
Xiong Y, Wakhloo AK, Fisher M. Advances in acute ischemic stroke therapy. Circ Res. 2022;130(8):1230-1251. doi: 10.1161/CIRCRESAHA.121.319948.
Abuelazm M, Seri AR, Awad AK, Ahmad U, Mahmoud A, Albazee E, et al. The efficacy and safety of tenecteplase versus alteplase for acute ischemic stroke: an updated systematic review, pairwise, and network meta-analysis of randomized controlled trials. J Thromb Thrombolysis. 2023;55(2):322-338. doi: 10.1007/s11239-022-02730-5. 7. Tsivgoulis G, Katsanos AH, Sandset EC, Turc G, Nguyen TN, Bivard A, et al. Thrombolysis for acute ischaemic stroke: current status and future perspectives. Lancet Neurol. 2023;22(5):418-429. doi: 10.1016/S1474-4422(22)00519-1
Cedillo-Reyes NA, Cuadra-Campos MC, Cosio-Mosqueira WA, Vásquez-Tirado GA. Eficacia de tenecteplase comparada con alteplase para tratamiento de ictus isquémico agudo: una revisión narrativa. Rev. chil. neuro-psiquiatr. [Internet]. 2023 [citado 2023 Nov 16];61(3):363-370. doi: 10.4067/s0717-92272023000300363
Gallardo-Tur A, Carazo-Barrios L, de la Cruz-Cosme C. Door-to-needle times for patients with ischaemic stroke treated with alteplase by on-site and off-site on-duty neurologists. PRISA study. Neurologia (Engl Ed). 2019;S0213-4853(19)30115-X. doi: 10.1016/j.nrl.2019.08.002
Iglesias Mohedano AM, García Pastor A, García Arratibel A, Sobrino García P, Díaz Otero F, Romero Delgado F, et al. Factors associated with in-hospital delays in treating acute stroke with intravenous thrombolysis in a tertiary centre. Neurologia. 2016;31(7): 452-8. doi: 10.1016/j.nrl.2014.12.004
Pulvers JN, Watson JDG. If Time is brain where is the improvement in prehospital time after stroke? Front Neurol. 2017;8:617. doi: 10.3389/fneur.2017.00617.
Iglesias Mohedano AM, García Pastor A, Díaz Otero F, Vázquez Alen P, Martín Gómez MA, Simón Campo P, et al. A new protocol reduces median door-to-needle time to the benchmark of 30 minutes in acute stroke treatment. Neurologia (Engl Ed). 2021;36(7): 487-494 . doi: 10.1016/j.nrleng.2018.03.009
González-Gómez FJ, Pérez-Torre P, DeFelipe A, Vera R, Matute C, Cruz-Culebras A, et al. Stroke in young adults: Incidence rate, risk factors, treatment and prognosis. Rev Clin Esp (Barc). 2016;216(7):345-351. doi: 10.1016/j.rce.2016.05.008
Scherle Matamoros CE, Rivero Rodríguez D, Di Capua Sacoto D, Maldonado Samaniego N, Mullo AE, Santacruz Villalba MJ, et al. Fibrinólisis Farmacológica En el ictus isquémico agudo: experiencia en un hospital terciario del Ecuador. Rev Ecuat Neurol [Internet]. 2019 [citado 2023 Nov 16]; 28(1):32-38. Disponible en: Disponible en: http://scielo.senescyt.gob.ec/scielo.php?script=sci_arttext&pid=S2631-25812019000100032&lng=es
Rey RC, Claverie CS, Alet MJ, Lepera SM, González LA. Manejo del accidente cerebrovascular en unidad especializada de un hospital público en el ámbito de la Ciudad de Buenos Aires y su relación con el sistema de atención médica de urgencias. Neurología Argentina.2018;10(4):225-231. doi: 10.1016/j.neuarg.2018.07.005
Gallo-Guerrero ML, Zevallos CB, Quiñones M. Factores asociados a resultados funcionales en pacientes con ictus isquémico tratados con trombolisis endovenosa en un hospital del Perú. Rev. Neuropsiquiatr. 2020 [citado 16 nov 2023];83(2):79-6. Disponible en: Disponible en: https://revistas.upch.edu.pe/index.php/RNP/article/view/3750/4179
Sánchez-Larsen A, García-García J, Ayo-Martín O, Hernández-Fernández F, Díaz-Maroto I, Fernández-Díaz E, et al. ¿Se ha producido un cambio en la etiología del ictus isquémico en las últimas décadas?: análisis y comparación de una base de datos de ictus actual frente a las históricas. Neurología. 2018;33(6):369-377. doi: 10.1016/j.nrl.2016.07.003
Vergara JP, Vera Vega O, Duran JP, Palacios Sánchez E, Gómez López A, Paba Gómez C. Caracterización del ataque cerebrovascular isquémico agudo en el servicio de urgencias. Repert Med Cir. 2023; 32(3): 253-260. doi: 10.31260/RepertMedCir.01217372.1067
Jauch EC, Saver JL, Adams HPJr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947. doi: 10.1161/STR.0b013e318284 056a
Tejada Meza H, Saldaña Inda I, Serrano Ponz M, Ara JR, Marta Moreno J. Impacto en los tiempos puerta-aguja de un conjunto de medidas para optimizar la atención hospitalaria del código ictus. Neurología. 2023;38(3):141-149. doi: 10.1016/j.nrl.2020.07.023
Murray CJL, Lopez AD. Measuring the global burden of disease. N Engl J Med . 2013;369(5): 448-57. doi: 10.1056/NEJMra1201534
Vicente-Pascual M, Quilez A, Gil MP, González-Mingot, Vázquez-Justes CD, Mauri-Capdevila G, et al. La influencia de la gestión organizativa en el tiempo puerta-aguja del tratamiento fibrinolítico. Neurología. 2023;38(5):313-318. doi: 10.1016/j.nrl.2020.10.014.
Guevara C, Bulatova K, Aravena F, Caba Sh, Monsalve J, Lara H, et al. Intravenous thrombolysis for ischemic stroke: experience in 54 patients. Rev. méd. Chile [Internet]. 2016 [citado 2023 Nov 15];144(4):434-441. doi: 10.4067/S0034-988720160004 00004
Brunser AM, Mazzon E, Muñoz P, Hoppe A, Lavados PM, Rojo A. et al. Determinantes del tiempo puerta-aguja en trombolisis endovenosa en el infarto cerebral, experiencia de un centro. Rev. méd. Chile [Internet]. 2020 [citado 2023 Nov 16]; 148(8):1090-1095. doi: 10.4067/S003498872020000801090
Fuentes B, Martínez-Sánchez P, Ruiz Ares G, Díez Tejedor E. Protocolo diagnóstico del ictus isquémico: estudios de imagen. Selección temporal. Medicine. 2015;11(71);4277-4281. doi: 10.1016/S0304-5412(15)30006-8
Vamsi V, Tekwani V, Ushakiranmayi V, Sikorskaa M. Resultados del tratamiento del ictus isquémico con y sin administración de terapia trombolítica: un estudio comparativo. Rev Cient Cienc Med 2018;21(1):30-39.
Cedeño Almeida LY, Neira García E, Olvera Arias A. Los Beneficios de la trombólisis con rt-pa en pacientes con evento cerebro vascular isquémico, según grupos de edad. Revista CYA [Internet]. 2023 [citado 15 de noviembre de 2023];2(1):1-21. Disponible en: Disponible en: https://revista.htmc.gob.ec/ojs-3.3.0-10/index.php/hetmc/article/view/26/60
Fernández López G. 2023. Administración de trombolíticos en pacientes con enfermedades cerebrovasculares isquémicas en Unidades de Cuidados Críticos. Revista Científica de Salud y Desarrollo Humano. 2023;4(2):85-102. doi: 10.61368/r.s.d.h.v4 i2.27