Mental disorders in children and adolescents with chronic kidney disease a first screening study conducted in Paraguay
Main Article Content
Abstract
Introduction: children and adolescents with chronic kidney disease often face unique challenges that significantly affect their mental well-being.
Objective: this study aimed to assess the mental health status of children and adolescents with CKD receiving care at the Pediatric Nephrology Department of the School of Medical Sciences of the Universidad Nacional de Asunción.
Methodology: this was a descriptive, prospective, cross-sectional observational study. We categorized participants based on sociodemographic factors (age, sex, residence, parents' marital status and education, and parental occupation) and clinical variables (age at chronic kidney disease diagnosis, underlying pathology, treatment type). Mental health assessments utilized the Brief Questionnaire for Screening and Diagnosis, adapted from Rutter's Child Scale. Diagnoses were classified as non-cases, probable uncomplicated cases, or definite complicated cases based on symptom severity.
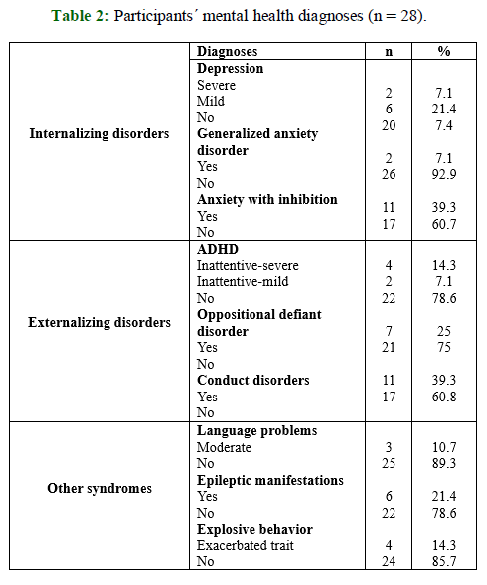
Results: our study analyzed 28 young individuals, predominantly male (57.1%), aged between 2 and 17 years with a mean age of 12.3 years. Approximately 42.9% hailed from the countryside, and half had parents who were divorced or separated. Clinically, 42.9% had chronic kidney disease stages I to III, 17.9% were at stage IV, and 39.3% had received kidney transplants. Mental health assessments via Brief Questionnaire for Screening and Diagnosis revealed that 39.3% did not show probable mental disorders, 32.1% were probable cases without complications, and 28.6% were probable cases with complications. Anxiety with inhibition and conduct disorders were the predominant disorders, each impacting 39.3% of participants.
Conclusion: our research underlines the significant burden of mental health disorders in a group of Paraguayan children and adolescents with chronic kidney disease and the pressing need for comprehensive, integrated mental health services that are specifically designed to meet the requirements of this vulnerable population.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Usted es libre de:
- Compartir: copiar y redistribuir el material en cualquier medio o formato para cualquier propósito, incluso comercialmente.
- Adaptar: remezclar, transformar y construir a partir del material para cualquier propósito, incluso comercialmente.
- La licenciante no puede revocar estas libertades en tanto usted siga los términos de la licencia
Bajo los siguientes términos:
- Atribución: Usted debe dar crédito de manera adecuada, brindar un enlace a la licencia, e indicar si se han realizado cambios. Puede hacerlo en cualquier forma razonable, pero no de forma tal que sugiera que usted o su uso tienen el apoyo de la licenciante.
- Compartir igual: — Si remezcla, transforma o crea a partir del material, debe distribuir su contribución bajo la misma licencia del original.
- No hay restricciones adicionales — No puede aplicar términos legales ni medidas tecnológicas que restrinjan legalmente a otras a hacer cualquier uso permitido por la licencia.
References
Gerson A, Wentz A, Abraham A, Mendley S, Hooper S, Butler R, et al. Health-related quality of life of children with mild to moderate chronic kidney disease. Pediatrics 2010;125(2):e349-e357. doi: 10.1542/peds.2009-0085.
Assadi F. Psychological impact of chronic kidney disease among children and adolescents: not rare and not benign. J Nephropathology 2013;2(1):1-3. doi: 10.5812/nephropathol.8968.
Verbitsky M, Kogon A, Matheson M, Hooper S, Wong C, Warady B, et al. Genomic disorders and neurocognitive impairment in pediatric CKD. J Am Soc Nephrol. 2017;28(8):2303-2309. doi: 10.1681/asn.2016101108.
Francis A, Didsbury M, Zwieten A, Chen K, James L, Kim S, et al. Quality of life of children and adolescents with chronic kidney disease: a cross-sectional study. Arch Dis Child. 2018;104(2):134-140. doi: 10.1136/archdischild-2018-314934.
Rodríguez Cuellar CI, García de la Puente S, Hernández Moraria J, Bojórquez Ochoa A, Filler G, Grishevich S. High depression rates among pediatric renal replacement therapy patients: a cross‐sectional study. Pediatr Transplantat. 2019;23(8):e13591. doi: 10.1111/petr.13591.
Erfidan G, Özyurt G, Özdemir-Şimşek Ö, Başaran C, Alaygut D, Mutlubaş F, et al. Is coronavirus pandemic‐related anxiety higher in children with chronic kidney disease than healthy children? Pediatrics International 2022;64(1):e14887. doi: 10.1111/ped.14887
Bakr A, Amr M, Sarhan A, Hammad A, Ragab M, El-Refaey A, et al. Psychiatric disorders in children with chronic renal failure. Pediatr Nephrol. 2007;22(1):128-31. doi: 10.1007/s00467-006-0298-9
Berney-Martinet S, Key F, Bell L, Lépine S, Clermont MJ, Fombonne E. Psychological profile of adolescents with a kidney transplant. Pediatr Transplant. 2009;13(6):701-10. doi: 10.1111/j.1399-3046.2008.01053.x.
Kogon AJ, Matheson MB, Flynn JT, Gerson AC, Warady BA, Furth SL, et al. Depressive symptoms in children with chronic kidney disease. J Pediatr. 2016;168:164-170.e1. doi: 10.1016/j.jpeds.2015.09.040.
Stahl JL, Wightman AG, Flythe JE, Weiss NS, Hingorani SR, Stoep AV. Psychiatric Diagnoses in Children With CKD Compared to the General Population. Kidney Med. 2022;4(6):100451. doi: 0.1016/j.xkme.2022.100451.
Torales J, Barrios I. Diseño de investigaciones: algoritmo de clasificación y características esenciales. Med. clín. soc.2023;7(3):210-235. doi: 10.52379/mcs.v7i3.349.
Caraveo-Anduaga JJ. Validez del Cuestionario Breve de Tamizaje y Diagnóstico (CBTD) para niños y adolescentes en escenarios clínicos. Salud mental. 2007;30(2):42-9. Disponible en: https://www.medigraphic.com/pdfs/salmen/sam-2007/sam072f.pdf
Zalai D, Szeifert L, Novák M. Psychological distress and depression in patients with chronic kidney disease. Seminars in Dialysis 2012;25(4):428-438. doi: 10.1111/j.1525-139x.2012.01100.x.
Lee K, Kim J, Hwang S, Cho N, Park S, Gil H, et al. The higher the CKD stage, the higher the psychological stress in patients with CKD during COVID-19 pandemic. J. Clin. Med. 2022;11(16):4776. doi: 10.3390/jcm11164776.
Marciano R, Soares C, Diniz J, Lima E, Silva J, Canhestro M, et al. Behavioral disorders and low quality of life in children and adolescents with chronic kidney disease. Pediatric Nephrology 2010;26(2):281-290. doi: 10.1007/s00467-010-1683-y.
Darwish A, Abdelnabi H. Sleep disorders in children with chronic kidney disease. International Journal of Pediatrics and Adolescent Medicine 2016;3(3):112-118. doi: 10.1016/j.ijpam.2016.06.001.
Gerson A, Butler R, Moxey-Mims M, Wentz A, Shinnar S, Lande M, et al. Neurocognitive outcomes in children with chronic kidney disease: current findings and contemporary endeavors. Ment Retard Dev Disabil Res Rev. 2006;12(3):208-215. doi: 10.1002/mrdd.20116
Xiong H, Zhang G, Wang L, Li Z, Shen Q, Li Y, et al. Psychological research of the children with chronic kidney disease and their guardians during the covid-19 pandemic. Front Public Health. 2022;10:1-11. doi: 10.3389/fpubh.2022.922678.
Senses Dinc G, Cak T, Cengel Kultur E, Bilginer Y, Kul M, Topaloglu R. Psychiatric morbidity and different treatment modalities in children with chronic kidney disease. Arch Pediatr. 2019;26(5):263-267. doi: 10.1016/j.arcped.2019.05.013.
Dryjańska N, Kiliś-Pstrusińska K. Depression in Children and Adolescents with Chronic Kidney Disease-Review of Available Literature. J Clin Med. 2023;12(10):3554. doi: 10.3390/jcm12103554.
Aier A, Pais P, Raman V. Psychological aspects in children and parents of children with chronic kidney disease and their families. Clin Exp Pediatr. 2022;65(5):222-229. doi: 10.3345/cep.2021.01004.