Enteral nutrition in critical ill patients with COVID-19 infection in mechanically ventilation with prone position
Main Article Content
Abstract
Introduction: SARS-CoV-2 since 2020 has generated countless challenges. Prone position was used to improve oxygenation, and nutritional therapy was adapted to meet requirements and reduce complications.
Objectives: evaluate the tolerance of enteral nutrition and its energetic adequacy in ventilated patients in the prone position with SARS-CoV-2 infection, in the respiratory room of the Adult Intensive Care Department of the Hospital de Clínicas - Facultad de Ciencias Médicas – Universidad Nacional de Asunción, from March to July 2021.
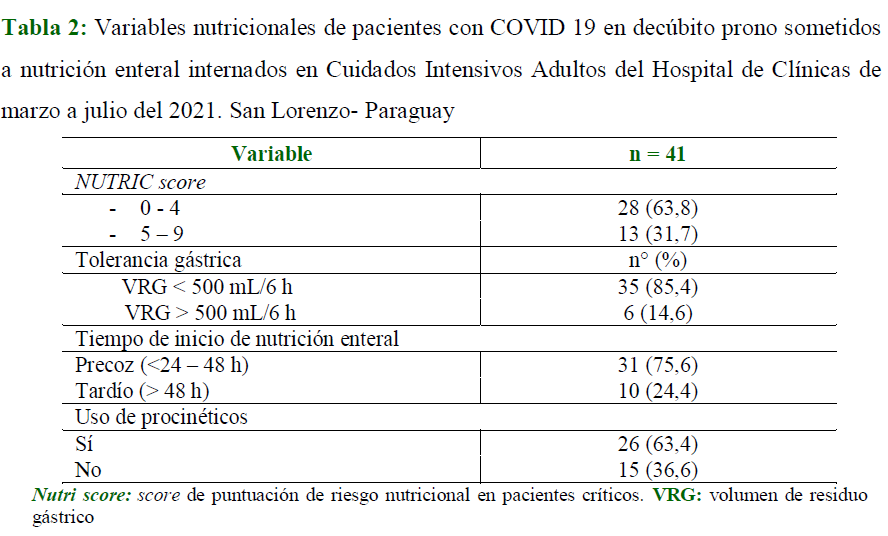
Methodology: observational, descriptive, retrospective, cross-sectional study of consecutive cases, with information obtained from records of intensive care patients, who received nutritional support in a prone position. Demographic, clinical and nutritional data were taken. Nutritional tolerance was evaluated during the prone position, defining it as the presence of a volume of gastric residue < 500 mL every 6 h. Energy adequacy was determined taking into account the percentage fulfilled of the nutritional prescription.
Results: 41 patients were recruited. 60.9 % were men; the median age was 55 years (IQR=23). The main comorbidities were obesity (57.3 %) and high blood pressure (43.9 %). 85.4 % had good gastric tolerance in the prone position, with gastric residue less than 500 ml. The percentage of energy adequacy was 84 %.
Conclusion: enteral nutritional therapy in the prone position was well tolerated by the majority of our patients, making it possible to achieve the indicated nutritional requirements.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Usted es libre de:
- Compartir: copiar y redistribuir el material en cualquier medio o formato para cualquier propósito, incluso comercialmente.
- Adaptar: remezclar, transformar y construir a partir del material para cualquier propósito, incluso comercialmente.
- La licenciante no puede revocar estas libertades en tanto usted siga los términos de la licencia
Bajo los siguientes términos:
- Atribución: Usted debe dar crédito de manera adecuada, brindar un enlace a la licencia, e indicar si se han realizado cambios. Puede hacerlo en cualquier forma razonable, pero no de forma tal que sugiera que usted o su uso tienen el apoyo de la licenciante.
- Compartir igual: — Si remezcla, transforma o crea a partir del material, debe distribuir su contribución bajo la misma licencia del original.
- No hay restricciones adicionales — No puede aplicar términos legales ni medidas tecnológicas que restrinjan legalmente a otras a hacer cualquier uso permitido por la licencia.
References
Moreira E, Olano E, Manzanares W. Terapia nutricional en el paciente crítico con COVID-19: una revisión. Rev. Méd. Urug. [Internet]. 2020 [cited 2023 May 08];36(4):102-130. doi: 10.29193/rmu.36.4.6.
Alencar ES de, Muniz LSDS, Holanda JLG, Oliveira BDD, Carvalho MCF de, Leitão AMM, et al. Enteral nutritional support for patients hospitalized with COVID-19: Results from the first wave in a public hospital. Nutrition [Internet]. 2022;94(111512):111512. doi: 10.1016/j.nut.2021.111512
Ellis B, Fuehne RJ. Examination of Accuracy in the Assessment of Gastric Residual Volume: A Simulated, Controlled Study. JPEN J Parenter Enteral Nutr [Internet]. 2015;39(4):434–40. doi: 10.1177/0148607114524230.
Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr [Internet]. 2019;38(1):48–79. doi: 10.1016/j.clnu.2018.08.037
Martindale R, Patel JJ, Taylor B, Warren M, Mcclave SA, McClave SA. Nutrition therapy in the patient with COVID-19 disease requiring ICU Care. 2020. Disponible en: https://www.nutritioncare.org/uploadedFiles/Documents/Guidelines_and_Clinical_Resources/COVID19/Nutrition%20Therapy%20in%20the%20Patient%20with%20COVID-19%20Disease%20Requiring%20ICU%20Care_Updated%20May%2026.pdf
Saez de la Fuente I, Saez de la Fuente J, Quintana Estelles MD, Garcia Gigorro R, Terceros Almanza LJ, Sanchez Izquierdo JA, et al. Enteral nutrition in patients receiving mechanical ventilation in a prone position. JPEN J Parenter Enteral Nutr [Internet]. 2016;40(2):250–5. doi: 10.1177/0148607114553232
Reignier J, Mercier E, Le Gouge A, Boulain T, Desachy A, Bellec F, et al. Effect of not monitoring residual gastric volumen risk of ventilator-associated pneumonia in adults receiving mechanical ventilation and early enteral feeding: a randomized controlled trial. JAMA [Internet]. 2013;309(3):249–56. doi: 10.1001/jama.2012.196377
Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Krznaric Z, Nitzan D, et al. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin Nutr [Internet]. 2020;39(6):1631–8. doi: 10.1016/j.clnu.2020.03.022
Campos LF, Barreto PA, Ceniccola GD, Gonçalves RC, de Matos LBN, Zambelli CMSF, et al. BRASPEN/AMIB recommendation for the confrontation of COVID-19 in hospitalized patients. BRASPEN J [Internet]. 2020;35(1):3-5. doi: 10.37111/braspenj.parecerbraspen2020
Matos AA, Sánchez Navas V, Quintero Villareal A, Méndez C, Petterson K, Vergara J, et al. Recommendations for nutritionas theraphy in critical patints with COVID-19. Acta Colomb Cuid Intensivo [Internet]. 2021;21(2):193–203. doi: 10.1016/j.acci.2021.01.002
Meléndez K, Vilcarromero A, Pillaca-Pullo O. La estratificación de la información por sexo en la COVID-19: un eslabón importante en la identificación de riesgos. Gac Sanit [Internet]. 2022;36(1):91–2. doi: 10.1016/j.gaceta.2020.12.032
Casas-Rojo JM, Antón-Santos JM, Millán-Núñez-Cortés J, Lumbreras-Bermejo C, Ramos-Rincón JM, Roy-Vallejo E, et al. Características clínicas de los pacientes hospitalizados con COVID-19 en España: resultados del Registro SEMI-COVID-19. Rev Clin Esp (Barc) [Internet]. 2020;220(8):480–94. doi: 10.1016/j.rce.2020.07.003
Serrano-Martínez JL, Machado-Casas JF, Redondo-Orts M, Manzano-Manzano F, Castaño-Pérez J, Pérez-Villares JM. Características y resultados de una serie de 59 pacientes con neumonía grave por COVID-19 ingresados en UCI. Med Intensiva (Engl Ed) [Internet]. 2020;44(9):580–3. doi: 10.1016/j.medin.2020.06.004
Savio RD, Parasuraman R, Lovesly D, Shankar B, Ranganathan L, Ramakrishnan N, et al. Feasibility, tolerance and effectiveness of enteral feeding in critically ill patients in prone position. J Intensive Care Soc [Internet]. 2021;22(1):41–6. doi: 10.1177/1751143719900100
Linn DD, Beckett RD, Foellinger K. Administration of enteral nutrition to adult patients in the prone position. Intensive Crit Care Nurs [Internet]. 2015;31(1):38–43. doi: 10.1016/j.iccn.2014.07.002
Alves de Paula J, Rabito EI, Justino SR, Leite LS, Dantas D, Makiyama da Silva JS, et al. Administration of enteral nutrition and gastrointestinal complications in Covid-19 critical patients in prone position. Clin Nutr Open Sci [Internet]. 2022;45:80–90. doi: 10.1016/j.nutos.2022.08.003
Jové Ponseti, E., Villarrasa Millán, A., & Ortiz Chinchilla, D. Análisis de las complicaciones del decúbito prono en el síndrome de distrés respiratorio agudo: estándar de calidad, incidencia y factores relacionados. Enfermeria Intensiva. 2017;28(3):125–134. doi: 10.1016/j.enfi.2016.12.003
Pereira Cunill JL, Martínez Ortega AJ, Gallego Casado C, García Luna PP. La medición del residuo gástrico en nutrición enteral. Nutr Clin En Medicina. 2016;X(2):108-21. doi: 10.7400/NCM.2016.10.2.5041
Galeano S, Castañeda Á, Guzmán E, Montoya M, Jaimes F. Deuda calórica en una cohorte de pacientes hospitalizados en unidades de cuidado intensivo. Rev Chil Nutr [Internet]. 2019;46(5):535–44. doi: 10.4067/s0717-75182019000500535
Heyland DK, Dhaliwal R, Wang M, Day AG. The prevalence of iatrogenic undernutrition in the nutritionally “at risk” critically ill patient: results of an international, multicenter, prospective study. Clin Nutr. 2015;34(4):659–66. doi: 10.1016/j.clnu.2014.07.008.
Álvarez J, Lallena S, Bernal M. Nutrition and the COVID-19 pandemic. Medicine [Internet]. 2020;13(23):1311–21. doi: 10.1016/j.med.2020.12.013
Ellis C, Brown M, Del Rosario KA, Heiden P, Salazar G, Sackey J, et al. A review of the tolerance and adequacy of enteral nutrition administered in the prone position in critically ill patients receiving mechanical ventilation. Curr Dev Nutr [Internet]. 2021;5(Suppl 2):216. doi: 10.1093/cdn/nzab029_017