Relationship between mouth breathing and malocclusion in children aged 6 to 12 years at the Enrique Solano López school, year 2023
Main Article Content
Abstract
Introduction: in Latin America, the prevalence of malocclusions, that is, alterations in the position and relationship of the teeth and jaws, reaches alarming levels and affects a high percentage of the children. Mouth breathing, a habit that deviates from the physiological pattern of nasal breathing, has become a public health problem. Worldwide, it is associated with the development of malocclusions, especially in children.
Methodology: this was a cross-sectional, descriptive and observational study. The sample size was 194 students. We evaluated the presence of mouth breathing, and malocclusion was classified according to Angle. The statistical program STATA 14.0 and the Chi-square test were used to determine the association between the variables.
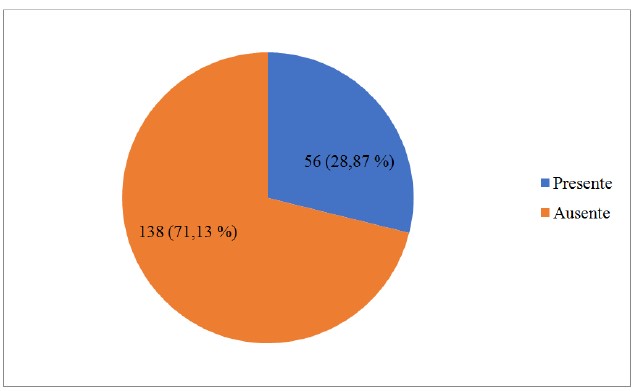
Results: the prevalence of mouth breathing was 28.87 %. Class I malocclusion was the most frequent (61.86 %), followed by Class II (25.77 %). A statistically significant association was found between mouth breathing and malocclusion (p=<0.001). The most frequent clinical signs in children with mouth breathing were: posterior crossbite with 58.9 %, ogival palate (80.4 %) and increased overjet/overbite (98.2 %).
Conclusions: there is a significant association between mouth breathing and malocclusion in the population studied. The prevalence of mouth breathing is similar to that reported in other Latin American studies.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Usted es libre de:
- Compartir: copiar y redistribuir el material en cualquier medio o formato para cualquier propósito, incluso comercialmente.
- Adaptar: remezclar, transformar y construir a partir del material para cualquier propósito, incluso comercialmente.
- La licenciante no puede revocar estas libertades en tanto usted siga los términos de la licencia
Bajo los siguientes términos:
- Atribución: Usted debe dar crédito de manera adecuada, brindar un enlace a la licencia, e indicar si se han realizado cambios. Puede hacerlo en cualquier forma razonable, pero no de forma tal que sugiera que usted o su uso tienen el apoyo de la licenciante.
- Compartir igual: — Si remezcla, transforma o crea a partir del material, debe distribuir su contribución bajo la misma licencia del original.
- No hay restricciones adicionales — No puede aplicar términos legales ni medidas tecnológicas que restrinjan legalmente a otras a hacer cualquier uso permitido por la licencia.
References
Grippaudo C, Paolantonio EG, Antonini G, Saulle R, La Torre G, Deli R. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngol Ital. 2016;36(5):386-394. doi: 10.14639/0392-100X-770.
Campanha SMA, Fontes MJF, Camargos PAM, Freire LMS. O impacto do tratamento fonoaudiológico no controle da asma e da rinite alérgica em crianças e adolescentes respiradores orais. J Pediatr (Rio J). 2010;86(3):202–8. Disponible en: https://www.scielo.br/j/jped/a/t8RdFBWmYBMgwmkk8wGH5bP/?format=pdf&lang=pt
Glupker L, Kula K, Parks, Babler W, Stewart K, Ghoneima A. Three-dimensional computed tomography analysis of airway volume changes between open and closed jaw positions. Am J Orthodontics dentofacial. 2015:147(4):426-434. doi: 10.1016/j.ajodo.2014.11.025.
Avrella M, Zimmermann R, Andriani P, Santos S, Barasuol J. Prevalence of anterior open bite in children and adolescents: a systematic review and meta-analysis. Eur Arch Paediatr Dent. 2022;23(3):355-364. doi: 10.1007/s40368-021-00683-6.
Valcheva Z, Arnautska H, Ivanova G, Atanasova I. Epidemiological research on the incidence of malocclusions among mouth-breathing children with primary and mixed dentition. Izvestia Journal of the Union of Scientists-Varna. Medicine and Ecology Series. 2018:23(1):127-133.
Kragt L, Dhamo B, Wolvius EB, Ongkosuwito EM. The impact of malocclusions on oral health-related quality of life in children-a systematic review and meta-analysis. Clin Oral Investig. 2016;20(8):1881-1894. doi: 10.1007/s00784-015-1681-3
Linder-Aronson S. Effects of adenoidectomy on dentition and nasopharynx. Trans Eur Orthod Soc. 1972:177-86.
Harvold EP, Tomer BS, Vargervik K, Chierici G. Primate experiments on oral respiration. Am J Orthod. 1981;79(4):359-72. doi: 10.1016/0002-9416(81)90379-1
McKeown P, Macalus, M. Mouth breathing: physical, mental and emotional consequences. Oral health. 2017. Disponible en: https://www.oralhealthgroup.com/features/mouth-breathing-physical-mental-emotional-consequences/
Triana G, Ali H, León G. Mouth breathing and its relationship to some oral and medical conditions: physiopathological mechanisms involved. Revista Habanera de CienciasMédicas. 2016: 15(2), 200-212.
Lin L, Zhao T, Qin D, Hua F, He H. The impact of mouth breathing on dentofacial development: A concise review. Front Public Health. 2022;10:929165.
Thilander B, Wahlund S. The prevalence of malocclusion in Swedish schoolchildren. Reseña de Scand J Dent. 1973;81(1):12-21. doi: 10.1111/j.1600-0722.1973.tb01489.x.
De Ridder L, Aleksieva A, Willems G, Declerck D, Cadenas de Llano-Pérula M. Prevalence of orthodontic malocclusions in healthy children and adolescents: a systematic review. Int J Environ Res Public Health. 2022;19(12):7446. doi: 10.3390/ijerph19127446
Kavaliauskienė A, Šidlauskas A, Žemaitienė M, Slabšinskienė E, Zaborskis A. Relationships of dental caries and malocclusion with oral health-related quality of life in lithuanian adolescents aged 15 to 18 years: a cross-sectional study. Int J Environ Res Public Health. 2020;17(11):4072. doi: 10.3390/ijerph17114072
Baskaradoss JK, Geevarghese A, Alsaadi W, Alemam H, Alghaihab A, Almutairi AS, et al. The impact of malocclusion on the oral health related quality of life of 11-14-year-old children. BMC Pediatr. 2022;22(1):91. doi: 10.1186/s12887-022-03127-2
Méndez J, Rotela R, González A. Prevalencia de Maloclusión en niños de 6 A 12 años de la ciudad de Coronel Oviedo, Paraguay, año 2016. Mem. Inst. Investig. Cienc. Salud. 2020;18(2):86-92. doi: 10.18004/mem.iics/1812-9528/2020.018.02.86
Mendoza P, Méndez J, Florentin D, Martínez G, Aguilar G, Ríos-González CM. Prevalencia de hábitos de succión no nutritiva y su relación con maloclusión y anomalías dentomaxilares en preescolares de Cnel. Oviedo, Paraguay. Mem. Inst. Investig. Cienc. Salud. 2019;17(3):49-54.
Silva Pérez A, Bulnes López M, Rodríguez López V. Prevalencia de hábito de respiración oral como factor etiológico de maloclusión en escolares del Centro, Tabasco. Revista ADM. 2014:71(6):285-289.
España P. Respiración bucal y maloclusión dentaria en niños de 6 a 10 años. Universidad de Guayaquil. Facultad de Odontología. 2019. Disponible en http://repositorio.ug.edu.ec/bitstream/redug/44166/1/ESPA%c3%91Apedro.pdf.
Vallejo E. La respiración bucal y su relación con la maloclusión dentaria. Universidad de Guayaquil. Facultad Pioloto de Odontología.; 2022. Disponible en http://repositorio.ug.edu.ec/bitstream/redug/60219/1/4150VALLEJOemily.pdf.
Cevallos L. Repiración bucal y desarrolo de maloclusiones.: Universidad de Guayaquil. Facultad de Odontología.; 2022. Disponible en http://repositorio.ug.edu.ec/bitstream/redug/63482/1/4206CEVALLOSlisseth.pdf
Abad M. Influencia de la respiración bucal en el desarrollo de los maxilares.: Universidad de Guayaquil. Facultad de Odontología.; 2022. Disponible en http://repositorio.ug.edu.ec/bitstream/redug/63964/1/4168ABADmaria.pdf.
Figueroa M. Hábitos bucales y maloclusión dentaria.: Universidad de Guayaquil. Facultad de Odontología.; 2020. Disponible en http://repositorio.ug.edu.ec/bitstream/redug/49785/1/3441FIGUEROAmauro.pdf.