Risk assessment of obstructive sleep apnea and adherence to pharmacological treatment in patients with arterial hypertension
Main Article Content
Abstract
Introduction: there is a suspicion about the bidirectional relationship between obstructive sleep apnea (OSA) and arterial hypertension (AHT). Both have a synergistic action on cardiovascular outcomes, so it is important to assess the prevalence of risk for OSA in hypertensive patients. In this last group we have also investigated the rate of adherence to prescribed drugs.
Metodology: through a case-control study and with the application of the STOP-BANG questionnaire, the risk categories for sleep apnea in the two cohorts have been discriminated. For the analysis of adherence to antihypertensive drugs, the abbreviated Morisky questionnaire was used.
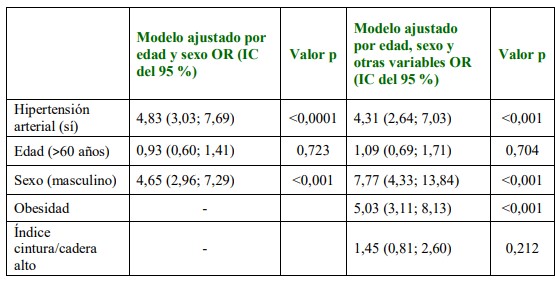
Results: 590 individuals were included (295 cases and 295 controls. A high risk for OSA was observed in the hypertensive group (36.6%) compared to 14.2% in the control group. On the other hand, the male sex OR 7.77 (95%CI 4.33-13.84), obesity OR 5.03 (95%CI 3.11-8.13) and hypertension OR 4.31 (95%CI 2.64-7.03) they are weighted significant in a logistic adjustment model studied here.61.69% of hypertensive patients reported adherence to the prescribed pharmacological treatment.
Discussion: OSA screening is feasible with a questionnaire applicable in daily clinical practice. From the pre-test clinical probability, specific diagnostic methods for the diagnosis of OSA must be started, emphasizing cases of resistant AHT, nocturnal AHT, and masked AHT. Local studies should be carried out to help us understand the causes of non-adherence to antihypertensive drugs in a significant fraction of individuals with AHT.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Usted es libre de:
- Compartir: copiar y redistribuir el material en cualquier medio o formato para cualquier propósito, incluso comercialmente.
- Adaptar: remezclar, transformar y construir a partir del material para cualquier propósito, incluso comercialmente.
- La licenciante no puede revocar estas libertades en tanto usted siga los términos de la licencia
Bajo los siguientes términos:
- Atribución: Usted debe dar crédito de manera adecuada, brindar un enlace a la licencia, e indicar si se han realizado cambios. Puede hacerlo en cualquier forma razonable, pero no de forma tal que sugiera que usted o su uso tienen el apoyo de la licenciante.
- Compartir igual: — Si remezcla, transforma o crea a partir del material, debe distribuir su contribución bajo la misma licencia del original.
- No hay restricciones adicionales — No puede aplicar términos legales ni medidas tecnológicas que restrinjan legalmente a otras a hacer cualquier uso permitido por la licencia.
References
Yusuf S, Joseph P, Rangarajan S, Islam Sh, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease and mortality in 155,722 individuals from 21 high-, middle-, and lowincome countries. Lancet. 2020; 395(10226): 795–808. doi:10.1016/S0140-6736(19)32008-2
Bozkurt B, Aguilar D, Deswal A, Dunbar SB, Francisco G, Horwich T, et al. Contributory risk and management of comorbidities of hypertension, obesity, diabetes mellitus, hyperlipidemia, and metabolic syndrome in chronic heart failure: a scientific statement from the american heart association. Circulation. 2016;134(23):e535–e578. doi: 10.1161/CIR.0000000000000450
Hall J, do Carmo JM, da Silva AA, Hall M. Obesity-Induced Hypertension: Interaction of Neurohumoral and Renal Mechanisms. Circ Res. 2015;116(6):991-1006. doi: 10.1161/CIRCRESAHA.116.305697
Jin ZN, Wei YX. Meta-analysis of effects of obstructive sleep apnea on the renin-angiotensinaldosterone system. J Geriatr Cardiol. 2016; 13(4): 333–343. doi:10.11909/j.issn.16715411.2016.03.020
Gottlieb D, Punjabi N. Diagnosis and management of obstructive sleep apnea a review. JAMA. 2020;323(14):1389-1400.doi:10.1001/jama.2020.3514
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Morrel MJ, Nunez CM, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019; 7(8): 687-698. doi: 10.1016/S2213-2600(19)30198-5
Yeghiazarins Y, Jneid H, Tietjens J, Redline S, Brown DL, El-Sherif N, et al. Obstructive Sleep Apnea and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021;144 (3): e56–e67. doi: 10.1161/CIR.0000000000000988
Bibbins-Domingo K, Grossman DC, Curry SJ. Screening for obstructive sleep apnea in adults: us preventive services task force recommendation statement. JAMA 2017 Jan 24;317(4):407-414.doi: 10.1001/jama.2016.20325. 9. Pulter N, Borghi C, Parati G, Pathak A, Toli D, Williams B, et al. Medication adherence in hypertension. J Hypertens. 2020;38(4):579-587. doi: 10.1097/HJH.0000000000002294
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg.. 2014;12(12:1500-24. doi: 10.1016/j.ijsu.2014.07.014.
Kales A, Bixler EO, Cadieux RJ, Schneck DW, Shaw LC, Locke TW, et al. Sleep apnoea in a hypertensive population. Lancet. 1984;2(8410):1005-8. doi:10.1016/s0140-6736(84)91107-3
Whelton PK, Carey RM, Aronow WS, Aronow W, Casey DE, Collins KJ, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/ AGS /APhA/ASH /ASPC/ NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online November 13, 2017]. Hypertension. 2018;71(6): e13-e115. doi:10.1161/HYP.0000000000000065
Chung F, Abdullah HR, Liao P. STOP-BANG Questionnaire: a practical approach to screen for obstructive sleep apnea. Chest. 2016; 149(3):631-8. doi: 10.1378/chest.15-0903.
Beyhaghi H, Reeve BB, Rodgers JE, Stearnes SC. Psychometric properties of the four-item Morisky Green levine medication adherence scale among atherosclerosis risk in communities (ARIC) study participants. Value Health. 2016;19(8):996-1001. doi: 10.1016/j.jval.2016.07.001.
World Health Organization; Waist circumference and waist-hip ratio: report of a WHO expert consultation. 2008. Ginebra: WHO. Acceso 30/11/2022. Disponible en: https://www.who.int/publications-detail-redirect/9789241501491
Kapur VK, Auckley DH, Chowdhuri S. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13(3):479-504. doi: 10.5664/jcsm.6506
Cherrez Ojeda I, Jeffe DB, Guerrero T. Attitudes and knowledge about obstructive sleep apnea among Latin American primary care physicians. Sleep Med. 2013;14(10):973-7. doi: 10.1016/j.sleep.2013.06.005
Blanco M, Ernst G, Valiensi S. Eficiencia del sueño en la polisomnografía nivel II de pacientes ambulatorios y hospitalizados. MEDICINA (Buenos Aires) 2020; 80: 317-323
Małolepsza A, Kudrycka A, Karwowska U. The role of screening questionnaires in the assessment of risk and severity of obstructive sleep apnea - polysomnography versus polygraphy. Adv Respir Med. 2021;89(2):188-196. doi: 10.5603/ARM.a2021.0038
Randerath W, Bassetti CL, Bonsignore MR. Challenges and perspectives in obstructive sleep apnoea: Report by an ad hoc working group of the Sleep Disordered Breathing Group of the European Respiratory Society and the European Sleep Research Society. Eur Respir J. 2018;52(3):1702616. doi: 10.1183/13993003.02616-2017
Silverberg DS, Oksenberg A, Iaina A. Sleep-related breathing disorders as a major causeof essential hypertension: fact or fiction. Curr Opin Nephrol Hypertens 1998; 7:353–357.
Fletcher EC, DeBehnke RD, Lovoi MS, Gorin AB. Undiagnosed sleep apnea in patientswith essential hypertension. Ann Intern Med 1985; 103: 190–195
Kareem O, Tanvir M, Bader G. Prevalence of high risk obstructive sleepapnoea by Berlin questionnaire in patientswith hypertension: study from a tertiarycare hospital. Sleep Science and Practice. 2020;4:15. doi.org/10.1186/s41606-020-00052-0.
González L, Castaño J, Herrera V. Relación entre hipertensión arterial y síndrome de apnea hipopnea obstructiva del sueño y sus factores de riesgo asociados, en población hipertensa de un centro médico de Cali (Colombia) 2008. ARCH. MED. (Manizales) 2008; 8 (2): 89-97
Hu FB, Willett WC, Colditz GA. Prospective study of snoring and risk of hypertension in women. Am J Epidemiol 1999;150:806-16
Peppard PE, Young T, Palt, Skatrud J. Prospective study of the association between sleepdisordered breathing and hypertension. N Engl J Med. 2000;342(19):1378-84. doi: 10.1056/NEJM200005113421901
Ren R, Covassin N, Yang L. Objective but not subjective short sleep duration is associated with hypertension in OSA. Hypertension 2018;72(3):610-617. doi: 10.1161/HYPERTENSIONAHA.118.11027
Cai A, Wang L, Zhou Y. Hypertension and obstructive sleep apnea. Hypertens Res. 2016;39(6):391-5. doi: 10.1038/hr.2016.11.
Carey RM, Calhoun DA, Bakris GL. Resistant hypertension: detection, evaluation, and management: a
cientific statement from the American Heart Association. Hypertension. 2018 ;72(5):e53-e90. doi:10.1161/HYP.0000000000000084
Calhoun DA, Nishizaka MK, Zaman MA. Aldosterone excretion amongsubjects with resistant hypertension and symptoms of sleep apnea. Chest 2004; 125:112–117. doi: 10.1378/chest.125.1.112
Pedrosa RP, Drager LF, Gonzaga CC. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811-7. doi:10.1161/HYPERTENSIONAHA.111.179788.
Loredo JS, Ancoli-Israel S, Dimsdale JE. Sleep quality and blood pressure dipping inobstructive sleep apnea. Am J Hypertens 2001; 14: 887–892.doi: 10.1016/s0895-7061(01)02143-4
Boggia J, Li Y, Thijs L, Hansen TW. Prognostic accuracy of day versus night ambulatory bloodpressure: a cohort study. Lancet 2007; 370(7): 1219–1229. doi: 10.1016/S01406736(07)61538-4
Baguet JP, Levy P, Barone-Rochette G. Masked hypertension in obstructive sleep apnea syndrome. J Hypertens2008; 26: 885–892. doi: 10.1097/HJH.0b013e3282f55049
Yeghiazarians Y, Jneid H, Tietjens JR. Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;144(3):e56-e67. doi:10.1161/CIR.0000000000000988.
Mitra, AK, Bhuiyan AR, Jones EA. Association and riskfactors for obstructive sleep apneaand cardiovascular diseases: asystematic review. Diseases 2021;9(4):88. doi.org/10.3390/diseases9040088
Bock JM, Rodysill KJ, Calvin AD. Waist-To-Hip Ratio Predicts Abnormal Overnight Oximetry in Men Independent of Body Mass Index. Front. Cardiovasc. Med. 2021; 8:789860. doi:10.3389/fcvm.2021.789860
Kunert J. Adherencia al tratamiento antihipertensivo en pacientes ambulatoriosde un hospital urbano. Rev. virtual Soc. Parag. Med. Int. 2015; 2 (2):43-51. doi:10.18004/rvspmi/23123893/2015.02(02)43-051
Zapatini D, Ortiz I. Adherencia terapéutica en pacientes hipertensos del consultorio de ClínicaMédica del Hospital de Clínicas. An. Fac. Cienc. Méd. (Asunción) 2021; 54 (2); 89-95. doi:10.18004/anales/2021.054.02.89
Vrijens B, Vincze G, Kristanto P. Adherence toprescribed antihypertensive drug treatments: longitudinal study of electronicallycompiled dosing histories. BMJ. 2008;336:1114–1117. doi:10.1136/bmj.39553.670231.25