Trastornos respiratorios del sueño en pacientes pediátricos atendidos en una clínica dental un estudio transversal
Contenido principal del artículo
Detalles del artículo

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Usted es libre de:
- Compartir: copiar y redistribuir el material en cualquier medio o formato para cualquier propósito, incluso comercialmente.
- Adaptar: remezclar, transformar y construir a partir del material para cualquier propósito, incluso comercialmente.
- La licenciante no puede revocar estas libertades en tanto usted siga los términos de la licencia
Bajo los siguientes términos:
- Atribución: Usted debe dar crédito de manera adecuada, brindar un enlace a la licencia, e indicar si se han realizado cambios. Puede hacerlo en cualquier forma razonable, pero no de forma tal que sugiera que usted o su uso tienen el apoyo de la licenciante.
- Compartir igual: — Si remezcla, transforma o crea a partir del material, debe distribuir su contribución bajo la misma licencia del original.
- No hay restricciones adicionales — No puede aplicar términos legales ni medidas tecnológicas que restrinjan legalmente a otras a hacer cualquier uso permitido por la licencia.
Citas
Piotto M, Gambadauro A, Rocchi A, Lelii M, Madini B, Cerrato L, et al. Pediatric Sleep Respiratory disorders: a narrative review of epidemiology and risk factors. Children (Basel). 2023;10(6):955. doi: 10.3390/children10060955.
Kaditis AG, Alonso Alvarez ML, Boudewyns A, Alexopoulos EI, Ersu R, Joosten K, et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J. 2016;47(1):69-94. doi: 10.1183/13993003.00385-2015.
Hansen C, Markström A, Sonnesen L. Sleep-disordered breathing and malocclusion in children and adolescents-a systematic review. J Oral Rehabil. 2022;49(3):353-361. doi: 10.1111/joor.13282.
Leibovitz S, Haviv Y, Sharav Y, Almoznino G, Aframian D, Zilberman U. Pediatric sleep-disordered breathing: role of the dentist. Quintessence Int. 2017;48(8):639-645. doi:10.3290/j.qi.a38554.
Katyal V, Pamula Y, Martin AJ, Daynes CN, Kennedy JD, Sampson WJ. Craniofacial and upper airway morphology in pediatric sleep-disordered breathing: systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2013;143(1):20-30.e3. doi: 10.1016/j.ajodo.2012.08.021.
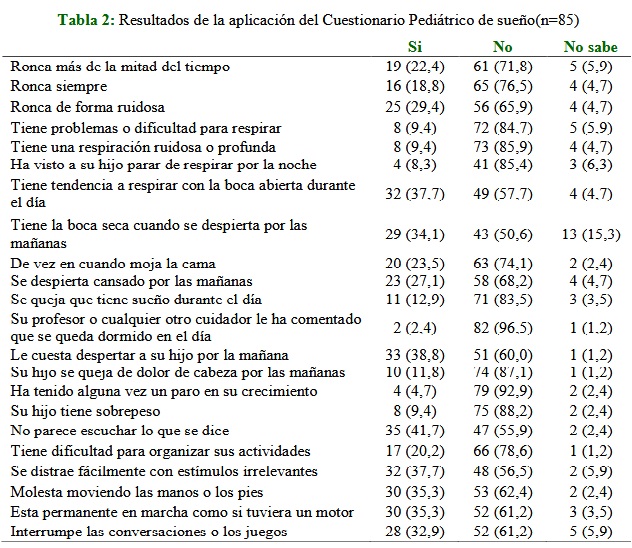
Chervin R, Hedger K, Dillon J, Pituch K. Pediatric sleep questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep medicine. 2000;1(1): 21-32. doi: 10.1016/s1389-9457(99)00009-x.
Vila M, Torres A, Soto B. Versión española del PediatricSleepQuestionnaire: un instrumento útil en la investigación de los trastornos del sueño en la infancia. Análisis de su fiabilidad. In Anales de pediatría. 2007; 66(2):121-128.
Gipson K, Lu M, Kinane TB. Sleep-disordered breathing in children. Pediatr Rev. 2019; 40(1):3-13. doi: 10.1542/pir.2018-0142. Erratum in: Pediatr Rev. 2019 May;40(5):261. doi: 10.1542/pir.405261.
Cho Y, Kwon Y, Ruth C, Cheng S, DelRosso LM. The burden of sleep disordered breathing in infants with Down syndrome referred to tertiary sleep center. PediatrPulmonol. 2023;58(4):1122-1126. doi: 10.1002/ppul.26302.
Aroucha Lyra MC, Aguiar D, Paiva M, Arnaud M, Filho AA, Rosenblatt A, et al. Prevalence of sleep-disordered breathing and associations with malocclusion in children. J Clin Sleep Med. 2020;16(7):1007-1012. doi: 10.5664/jcsm.8370.
Pérez Bejarano NM, GuggiariNiederberger AL, OtazúCambiano AA. Trastornos respiratorios relacionados al sueño en niños que acuden a la consulta ortodóncica en el Instituto de Odontología Avanzada, Paraguay 2018. Rev. salud pública Parag. 2019;9(2):16-21. Disponible en: https://revistas.ins.gov.py/index.php/rspp/article/view/21/21
Tsuda H, Fastlicht S, Almeida FR, Lowe AA. The correlation between craniofacial morphology and sleep-disordered breathing in children in an undergraduate orthodontic clinic. Sleep Breath. 2011;15(2):163-71. doi: 10.1007/s11325-010-0345-4.
Iwasaki T, Yamasaki Y. Relation between maxillofacial form and respiratory disorders in children. Sleep and Biologica Rhythms. 2014;12(1): 2-11. doi: 10.1111/sbr.12041
Gouthro K, Slowik JM. Pediatric obstructive sleep apnea. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Disponible en: https://www.ncbi.nlm.nih.gov/books/NBK557610/
Bonuck K, Freeman K, Chervin RD, Xu L. Sleep-disordered breathing in a population-based cohort: behavioral outcomes at 4 and 7 years. Pediatrics. 2012;129(4):e857-65. doi: 10.1542/peds.2011-1402.
Chan J, Edman JC, Koltai PJ. Obstructive sleep apnea in children. Am Fam Physician. 2004;69(5):1147-54.
Jackman AR, Biggs SN, Walter LM, Embuldeniya US, Davey MJ, Nixon GM, et al. Sleep-disordered breathing in preschool children is associated with behavioral, but not cognitive, impairments. Sleep Med. 2012;13(6):621-31. doi: 10.1016/j.sleep.2012.01.013.
Gozal D, Kheirandish-Gozal L. Neurocognitive and behavioral morbidity in children with sleep disorders. CurrOpinPulm Med.
;13(6):505-9. doi: 10.1097/MCP.0b013e3282ef6880.
Walter LM, Shepherd KL, Yee A, Horne RSC. Insights into the effects of sleep disordered breathing on the brain in infants and children: imaging and cerebral oxygenation measurements. Sleep Med Rev. 2020;50:101251. doi: 10.1016/j.smrv.2019.101251.
Chervin RD, Weatherly RA, Garetz SL, Ruzicka DL, Giordani BJ, Hodges EK, et al. Pediatric sleep questionnaire: prediction of sleep apnea and outcomes. Arch Otolaryngol Head Neck Surg. 2007;133(3):216-22. doi: 10.1001/archotol.133.3.216.
Rundo JV, Downey R 3rd. Polysomnography. Handb Clin Neurol. 2019;160:381-392. doi: 10.1016/B978-0-444-64032-1.00025-4.
American Academy of Pediatric Dentistry. Management of the developing dentition and occlusion in pediatric dentistry. The Reference Manual of Pediatric Dentistry. Chicago, Ill: American Academy of Pediatric Dentistry; 2017. 388-405 p.
Guilleminault C, Akhtar F. Pediatric sleep-disordered breathing: new evidence on its development. Sleep Med Rev. 2015;24:46-56. doi: 10.1016/j.smrv.2014.11.008