Medical professionalism in clinical and surgical specialties an analysis of Latin American physicians
Main Article Content
Abstract
Introduction: professionalism is crucial in medical practice and can vary by specialty. Factors such as ethical behavior and commitment to continuing education influence professional performance.
Objective: to identify behaviors associated with professionalism that differentiate clinical and surgical specialist physicians.
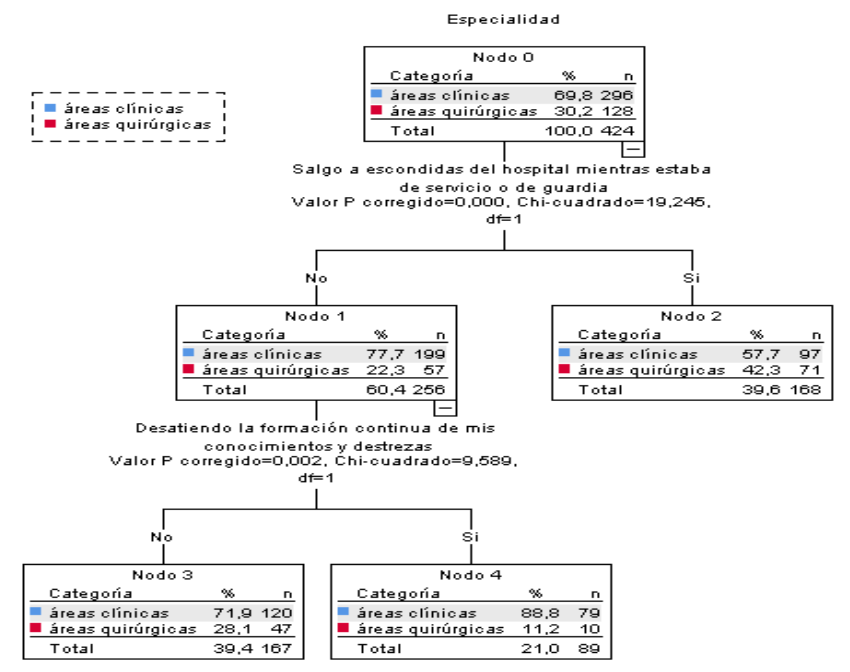
Methodology: 424 physicians from Peru, Paraguay, and Cuba were evaluated and classified intoclinical (n =296) and surgical (n=128) specialties. The CHAID (Chi-squared Automatic Interaction Detection) method was applied with 43 indicators and 7 dimensions to identify predictors of professionalism.
Results: the CHAID analysis showed significant differences between specialties. Themost influential variable was “I sneak out of the hospital while on duty” (p<0.001), with a higher representation of clinical specialist physicians who never did this (77.70 %) compared to surgical specialists (22.30 %), with means of 1.13 versus 1.31, respectively. The variable “neglecting continuing education” (p=0.002) showed that more clinical specialist physicians did not neglect their training (71.90%) with a mean of 1.14, while those who did so reached 88.8 % (surgical: 11.2 %) with a mean of 1.28. In the dimensions “dishonesty and unsafe practice” and “irresponsible conduct and disabilities”, physicians with negative behaviors had higher means (1.36 and 1.29) than those without these practices (1.13 and 1.10).
Conclusions: the CHAID analysis revealed key differences in medical professionalism by specialty, associating the absence of negative behaviors and commitment to continuing education with higher levels of professionalism, especially in clinical specialist physicians.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Usted es libre de:
- Compartir: copiar y redistribuir el material en cualquier medio o formato para cualquier propósito, incluso comercialmente.
- Adaptar: remezclar, transformar y construir a partir del material para cualquier propósito, incluso comercialmente.
- La licenciante no puede revocar estas libertades en tanto usted siga los términos de la licencia
Bajo los siguientes términos:
- Atribución: Usted debe dar crédito de manera adecuada, brindar un enlace a la licencia, e indicar si se han realizado cambios. Puede hacerlo en cualquier forma razonable, pero no de forma tal que sugiera que usted o su uso tienen el apoyo de la licenciante.
- Compartir igual: — Si remezcla, transforma o crea a partir del material, debe distribuir su contribución bajo la misma licencia del original.
- No hay restricciones adicionales — No puede aplicar términos legales ni medidas tecnológicas que restrinjan legalmente a otras a hacer cualquier uso permitido por la licencia.
References
Bhardwaj A. Medical professionalism in the provision of clinical care in health care organizations. J Healthc Leadersh [Internet]. 2022;14:183–9. doi: 10.2147/jhl.s383069.
Kirk LM. Professionalism in medicine: Definitions and considerations for teaching. Proc (Bayl Univ Med Cent) [Internet]. 2007;20(1):13–6. doi: 10.1080/08998280.2007.11928225.
Desai MK, Kapadia JD. Medical professionalism and ethics. J Pharmacol Pharmacother [Internet]. 2022;13(2):113–8. doi: 10.1177/0976500x221111448.
Rosen MA, Diaz Granados D, Dietz AS, Benishek LE, Thompson D, Pronovost PJ, et al. Teamwork in healthcare: Key discoveries enabling safer, high-quality care. Am Psychol [Internet]. 2018;73(4):433–50. Disponible en: doi: 10.1037/amp0000298.
ABIM Foundation, ACP-ASIM Foundation, European Federation of Internal Medicine. Medical professionalism in the new millennium: a physician charter. Ann Intern Med [Internet]. 2002;136(3):243–6. Disponible en: doi: 10.7326/0003-4819-136-3-200202050-00012
Royal College of Physicians. Doctors in society: medical professionalism in a changing world [Internet]. RCP London. 2005. Disponible en: https://shop.rcp.ac.uk/products/doctors-in-societymedical-professionalism-in-a-changing-world?variant=6337443013
American Board of Pediatrics. Guide to professionalism in pediatrics. Chapel Hill: ABP; 2012. Disponible en: https://www.abp.org/sites/abp/files/pdf/professionalism.pdf
Varkey B. Principles of clinical ethics and their application to practice. MedPrincPract [Internet]. 2021;30(1):17–28. Disponible en: doi: 10.1159/000509119
Madzia JL. “To be professional, it isn’t necessarily our full selves”: How medical students with minoritized identities manage tensions between medical professionalism and their own professional identities. SSM Qual Res Health [Internet]. 2023;4(100313):100313. doi: 10.1016/j.ssmqr.2023.100313
Arantzamendi M, Sapeta P, Belar A, Centeno C. How palliative care professionals develop coping competence through their career: a grounded theory. Palliat Med [Internet]. 2024;38(3):284–96. doi: 10.1177/02692163241229961
Øyri SF, Wiig S, Tjomsland O. Influence of external assessment on quality and safety in surgery: a qualitative study of surgeons’ perspectives. BMJ Open Qual [Internet]. 2024;13(2):e002672. doi:10.1136/bmjoq-2023-002672
Chang H-J, Lee Y-M, Lee Y-H, Kwon H-J. Investigation of unethical and unprofessional behavior in Korean residency training. Teach Learn Med [Internet]. 2015;27(4):370–8. doi: 10.1080/10401334.2015.1077128
Choi H-Y, Kim E-Y, Kim J. Prognostic factors in diabetes: comparison of Chi-square automatic interaction detector (CHAID) decision tree technology and logistic regression. Medicine (Baltimore) [Internet]. 2022;101(42):e31343. doi: 10.1097/md.0000000000031343
Muñoz-Rodríguez JM, Patino Alonso C, Pessoa T, Martín-Lucas J. Identity profile of young people experiencing a sense of risk on the internet: a data mining application of decision tree with CHAID algorithm. Comput Educ [Internet]. 2023;197(104743):104743. doi:10.1016/j.compedu.2023.104743
Świtalski J, Wnuk K, Tatara T, Miazga W, Wiśniewska E, Banaś T, et al. Interventions to increase patient safety in long-term care facilities—umbrella review. Int J Environ Res Public Health [Internet]. 2022;19(22):15354. doi: 10.3390/ijerph192215354
Neyens DM, Bayramzadeh S, Catchpole K, Joseph A, Taaffe K, Jurewicz K, et al. Using a systems approach to evaluate a circulating nurse’swork patterns and work flow disruptions. Appl Ergon [Internet]. 2019;78:293–300. doi: 10.1016/j.apergo.2018.03.017
Tokuç B, Varol G. Medical education in the era of advancing technology. Balkan Med J [Internet]. 2023;40(6):395–9. doi: 10.4274/balkanmedj.galenos.2023.2023-7-79
Odero A, Pongy M, Chauvel L, Voz B, Spitz E, Pétré B, et al. Core values that influence the patient—health care professional power dynamic: steering interaction to wards partner ship. Int J Environ Res Public Health [Internet]. 2020;17(22):8458. doi: 10.3390/ijerph17228458
Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R. The impact of stress on surgical performance: a systematic review of the literature. Surgery [Internet]. 2010;147(3):318-330.e6. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S0039606009006175