Autolesiones no suicidas en estudiantes de medicina frecuencia y factores asociados
Contenido principal del artículo
Resumen
Introducción: la salud mental de los estudiantes de medicina ha sido ampliamente investigada, demostrando que forman parte de un grupo vulnerable al desarrollo de trastornos mentales.
Objetivo: el objetivo de esta investigación fue determinar la frecuencia de NSSI y sus factores asociados en estudiantes de medicina del Paraguay.
Metodología: este fue un estudio descriptivo y transversal. Se lanzó una encuesta online para evaluar depresión, ansiedad y autolesiones, se utilizaron las escalas PHQ-2, GAD-7 y SHQ, respectivamente.
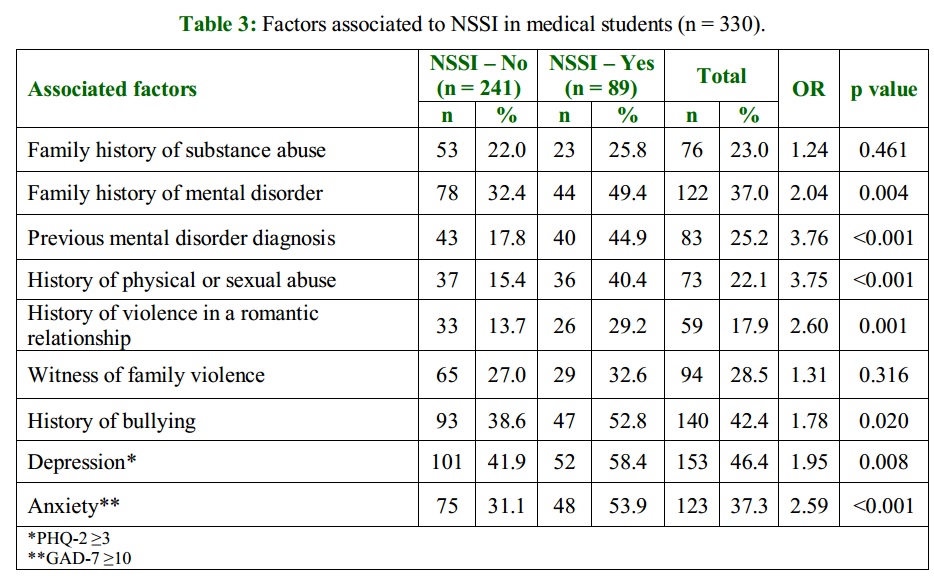
Resultados: recibimos respuestas de 330 estudiantes de medicina. De los participantes, el 71,2 % eran mujeres. Se identificó que el 46,4 % de los participantes padecía depresión (PHQ-2 ≥ 3) y el 37,3 % ansiedad (GAD-7 ≥10). La frecuencia de NSSI fue del 27 % (n = 89). Los principales factores asociados a NSSI fueron un diagnóstico previo de un trastorno mental (que aumentó la probabilidad de NSSI en 3,76 veces) y/o una historia de abuso físico o sexual (con un aumento de 3,75 veces).
Conclusión: esta investigación encontró la presencia de NSSI en casi 3 de cada 10 de los estudiantes de medicina encuestados. Los principales factores asociados con la conducta autolesiva fueron un diagnóstico previo de un trastorno mental y/o antecedentes de abuso físico o sexual.
Detalles del artículo

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Usted es libre de:
- Compartir: copiar y redistribuir el material en cualquier medio o formato para cualquier propósito, incluso comercialmente.
- Adaptar: remezclar, transformar y construir a partir del material para cualquier propósito, incluso comercialmente.
- La licenciante no puede revocar estas libertades en tanto usted siga los términos de la licencia
Bajo los siguientes términos:
- Atribución: Usted debe dar crédito de manera adecuada, brindar un enlace a la licencia, e indicar si se han realizado cambios. Puede hacerlo en cualquier forma razonable, pero no de forma tal que sugiera que usted o su uso tienen el apoyo de la licenciante.
- Compartir igual: — Si remezcla, transforma o crea a partir del material, debe distribuir su contribución bajo la misma licencia del original.
- No hay restricciones adicionales — No puede aplicar términos legales ni medidas tecnológicas que restrinjan legalmente a otras a hacer cualquier uso permitido por la licencia.
Citas
Carrieri D, Pearson M, Mattick K, Papoutsi C, Briscoe S, Wong G, et al. Interventions to minimise doctors’ mental ill-health and its impacts on the workforce and patient care: the care under pressure realist review. Health Serv Deliv Res NIHR. 2020;8(19): 1-132. doi: 10.3310/hsdr08190.
Barrios I, Miltos V, Piris A, Piris G, Ramírez C, Rodríguez J, et al. Tamizaje de salud mental mediante el test M.I.N.I. en estudiantes del ciclo básico de medicina de la Universidad Nacional de Asunción. An Fac Cienc Médicas. 2015;48(1):59-68.
Torales J, Kadhum M, Zárate G, Barrios I, González I, Farrell SM, et al. Wellbeing and mental health among medical students in Paraguay. Int Rev Psychiatry. 2019;31(7-8):598-602.
Castaldelli-Maia JM, Lewis T, Marques Dos Santos N, Picon F, Kadhum M, Farrell SM, et al. Stressors, psychological distress, and mental health problems amongst Brazilian medical students. Int Rev Psychiatry Abingdon Engl. 2019;31(7-8):603-7.
Almeida T, Kadhum M, Farrell SM, Ventriglio A, Molodynski A. A descriptive study of mental health and wellbeing among medical students in Portugal. Int Rev Psychiatry Abingdon Engl. 2019;31(7-8):574-8.
Awad F, Awad M, Mattick K, Dieppe P. Mental health in medical students: time to act. Clin Teach. 2019;16(4):312-6.
Chau SWH, Lewis T, Ng R, Chen JY, Farrell SM, Molodynski A, et al. Wellbeing and mental health amongst medical students from Hong Kong. Int Rev Psychiatry Abingdon Engl. 2019;31(7-8):626-9.
Masri R, Kadhum M, Farrell SM, Khamees A, Al-Taiar H, Molodynski A. Wellbeing and mental health amongst medical students in Jordan: a descriptive study. Int Rev Psychiatry Abingdon Engl. 2019;31(7-8):619-25.
Molodynski A, Lewis T, Kadhum M, Farrell SM, Lemtiri Chelieh M, Falcão De Almeida T, et al. Cultural variations in wellbeing, burnout and substance use amongst medical students in twelve countries. Int Rev Psychiatry. 2021;33(1-2):37-42.
Hawton K, Saunders KEA, O’Connor RC. Self-harm and suicide in adolescents. Lancet Lond Engl. 2012;379(9834):2373-82.
American Psychiatric Association. Manual diagnóstico y estadístico de los trastornos mentales: DSM-5. Buenos Aires: Editorial Médica Panamericana; 2019.
Nock MK. Self-Injury. Annu Rev Clin Psychol. 2010;6(1):339-63.
Klonsky ED, Muehlenkamp JJ. Self-injury: a research review for the practitioner. J Clin Psychol. 2007;63(11):1045-56.
Mollà L, Batlle Vila S, Treen D, López J, Sanz N, Martín LM, et al. Autolesiones no suicidas en adolescentes: revisión de los tratamientos psicológicos. Rev Psicopatología Psicol Clínica. 2015;20(1):51-61.
Royal College of Psychiatrists. Self-harm, suicide and risk: helping people who self-harm Final report of a working group. College Report CR158 [Internet]. London; 2010. Available from: https://www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/college-reports/college-report-cr158.pdf?sfvrsn=fcf95b93_2
García-Mijares JF, Alejo-Galarza G de J, Mayorga-Colunga SR, Guerrero-Herrera LF, Ramírez-GarcíaLuna JL, García-Mijares JF, et al. Validación al español del Self-Harm Questionnaire para detección de autolesionismo en adolescentes. Salud Ment. 2015;38(4):287-92.
Krantz JH, Dalal R. Validity of Web-Based Psychological Research. In: Psychological Experiments on the Internet. Elsevier; 2000. p. 35-60.
Gosling SD, Vazire S, Srivastava S, John OP. Should We trust web-based studies? a comparative analysis of six preconceptions about internet questionnaires. Am Psychol. 2004;59(2):93-104.
Allroggen M, Kleinrahm R, Rau TAD, Weninger L, Ludolph AG, Plener PL. Nonsuicidal self-injury and its relation to personality traits in medical students. J Nerv Ment Dis. 2014;202(4):300-4.
Kroenke K, Spitzer RL, Williams JBW. The Patient health questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284-92.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-13.
Torales J, Barrios I, Ayala N, O’Higgins M, Palacios JM, Ríos-González C, et al. Ansiedad y depresión en relación a noticias sobre COVID-19: un estudio en población general paraguaya. Rev Salud Publica Parag. 2021;11(1):67-73.
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A Brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092.
Forrester RL, Slater H, Jomar K, Mitzman S, Taylor PJ. Self-esteem and non-suicidal self-injury in adulthood: a systematic review. J Affect Disord. 2017;221:172-83. doi: 10.1016/j.jad.2017.06.027.
Ougrin D, Boege I. Brief report: the self harm questionnaire: a new tool designed to improve identification of self harm in adolescents. J Adolesc. 2013;36(1):221-5.
Meszaros G, Horvath LO, Balazs J. Self-injury and externalizing pathology: a systematic literature review. BMC Psychiatry. 2017;17(1):160.
Donath C, Bergmann MC, Kliem S, Hillemacher T, Baier D. Epidemiology of suicidal ideation, suicide attempts, and direct self-injurious behavior in adolescents with a migration background: a representative study. BMC Pediatr. 2019;19:45.
Coppersmith DDL, Nada-Raja S, Beautrais AL. Non-Suicidal self-injury and suicide attempts in a New Zealand birth cohort. J Affect Disord. 2017;221:89-96.
Zeng W, Chen R, Wang X, Zhang Q, Deng W. Prevalence of mental health problems among medical students in China: a meta-analysis. Medicine (Baltimore). 2019;98(18):e15337.
Pacheco JP, Giacomin HT, Tam WW, Ribeiro TB, Arab C, Bezerra IM, et al. Mental health problems among medical students in Brazil: a systematic review and meta-analysis. Rev Bras Psiquiatr. 2017;39(4):369-78
Wang Y, Zhao Y, Liu L, Chen Y, Ai D, Yao Y, et al. The current situation of internet addiction and its impact on sleep quality and self-injury behavior in chinese medical students. Psychiatry Investig. 2020;17(3):237-42.
Wu D, Rockett IRH, Yang T, Feng X, Jiang S, Yu L. Deliberate self-harm among Chinese medical students: a population-based study. J Affect Disord. 2016;202:137-44.
Kaparounaki CK, Patsali ME, Mousa DPV, Papadopoulou EVK, Papadopoulou KKK, Fountoulakis KN. University students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020;290:113111.
Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317-20.
Gentile A, Torales J, O’Higgins M, Figueredo P, Castaldelli-Maia JM, De Berardis D, et al. Phone-based outpatients’ follow-up in mental health centers during the COVID-19 quarantine. Int J Soc Psychiatry. 2022;68(1):129-133.
Selenius H, Strand S. Experiences of self-injury and aggression among women admitted to forensic psychiatric care. Nord J Psychiatry. 2017;71(4):304-11
Parker G, Malhi G, Mitchell P, Kotze B, Wilhelm K, Parker K. Self-harming in depressed patients: pattern analysis. Aust N Z J Psychiatry. 2005;39(10):899-906.
Law GU, Rostill-Brookes H, Goodman D. Public stigma in health and non-healthcare students: attributions, emotions and willingness to help with adolescent self-harm. Int J Nurs Stud. 2009;46(1):107-18.
Alexander Arguello P, Addington A, Borja S, Brady L, Dutka T, Gitik M, et al. From genetics to biology: advancing mental health research in the Genomics ERA. Mol Psychiatry. 2019;24(11):1576-82.
Vega D, Sintes A, Fernández M, Puntí J, Soler J, Santamarina P, et al. Review and update on non-suicidal self-injury: who, how and why? Actas Esp Psiquiatr. 2018;46(4):146-55.
Maniglio R. The role of child sexual abuse in the etiology of suicide and non-suicidal self-injury. Acta Psychiatr Scand. 2011;124(1):30-41.
Kiekens G, Hasking P, Claes L, Boyes M, Mortier P, Auerbach RP, et al. Predicting the incidence of non-suicidal self-injury in college students. Eur Psychiatry. 2019;59:44-51.
Kapur N, Gask L. Introduction to suicide and self-harm. Psychiatry. 2009;8(7):233-6.
Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316(21):2214-36.
Menon P, Chaudhury S, Saldanha D, Sahu S, Singh V, Pathak V. Stress levels and its association with self-harm and risk-taking behavior in medical undergraduates. Ind Psychiatry J. 2018;27(1):41.
Goebert D, Thompson D, Takeshita J, Beach C, Bryson P, Ephgrave K, et al. Depressive symptoms in medical students and residents: a multischool study. Acad Med J Assoc Am Med Coll. 2009;84(2):236-41
Thompson D, Goebert D, Takeshita J. A program for reducing depressive symptoms and suicidal ideation in medical students. Acad Med J Assoc Am Med Coll. 2010;85(10):1635-9.
MacArthur KR, Koley J, Wengel SP. Student Perceptions of a reflective writing-based wellness course: ‘good in theory, but...’ Med Sci Educ. 2021;31(3):1043-51.
Watson C, Ventriglio A, Bhugra D. A narrative review of suicide and suicidal behavior in medical students. Indian J Psychiatry. 2020;62(3):250-6.
Nikolis L, Wakim A, Adams W, Do PB. Medical student wellness in the United States during the COVID-19 pandemic: a nationwide survey. BMC Med Educ. 2021;21(1):401.
Heinen I, Bullinger M, Kocalevent RD. Perceived stress in first year medical students - associations with personal resources and emotional distress. BMC Med Educ. 2017;17(1):4